9 Surprising Things We Don’t Do When Treating OCD at Our Clinic
Photo by: photographee.eu / Sthutterstock.com
If you have OCD, you have probably read numerous blog posts and books about the treatment strategies for OCD. Maybe you even went to therapy.
It is very likely that in the process of seeking OCD treatment you have become disillusioned as the suggested strategies haven’t worked for you. This may have happened even if you went to see a therapist that practices using the Cognitive Behavioural Therapy (CBT) framework.
When patients call us to inquire about our services, they often say that they tried CBT and it hasn’t been useful to them at all. Moreover, some feel that it created even more obsessions and compulsions and their psychological state worsened.
CBT is the recommended evidence-based approach to the treatment of OCD. How come, then, it hasn’t been helpful to all these people?
The problem is that not all CBT techniques work for OCD. They may work for mild to moderate anxiety, but OCD requires a very specialized approach. It is called Exposure and Response Prevention (ERP or ExRP). This approach is strongly rooted in CBT, but it is an approach by itself nevertheless, and CBT techniques are used in a different way within ERP.
Moreover, even ERP has changed in recent years. If you have tried Exposure therapy in the past, you may be surprised reading the following list of the strategies that we do not use as your exposure therapist may have encouraged you to use them in the past.
One example of exposure therapy done “the old way” is Systematic Desensitization. This is an older behavioural intervention that some therapists are still using to address compulsions. It includes very gradual exposure to OCD triggers and is combined with relaxation techniques that are used to control anxiety. The goal is to lower anxiety and to approach the feared trigger in a relaxed state. As you have probably figured out on your own the hard way, the attempts to reduce anxiety may successfully diminish it for a short period, but it always comes back. Also, this technique implies that you can only do exposure (that is, face your fears) when you are relatively calm, which is not true: you can be very anxious and face your fears anyway.
Another example is concentrating on rating anxiety and aiming to reduce it during the exposure. This usually includes rating and re-rating your SUDs (Subjective Units of Distress) and gearing the exposure toward reducing them in half. Similar to the previous example, again the focus here is on anxiety reduction, which in itself creates struggle and unnecessary suffering.
Here are 9 things that you might have done in OCD therapy before that are mostly ineffective for OCD treatment:
1. Exploring Childhood and Teen Issues that Might have Caused OCD
It may be tempting to both the therapist and the patient to try and uncover the “real root of OCD” through lengthy discussions, then focus on attachment and childhood relationships and experiences. It seems that if you finally figure out what the initial OCD cause was, then the problem will be resolved.
This quest for uncovering childhood experiences is further reinforced by the fact that in many cases, OCD does seem to be triggered by a certain experience.
Some case examples:
When Dan was nine years old, he was hospitalized with salmonellosis. At discharge, his doctor urged him to wash his hands really well to avoid getting bacterial poisoning in the future. This was the start of his compulsive washing that worsened throughout the years.
Helen remembers a pastor at her church talking about bad people going to hell. She came home that day and recited extra prayers. After that she felt the urge to ask her parents repeatedly if she was a good girl and ask for forgiveness just in case she wasn’t. The praying and asking for forgiveness gradually became excessive and time-consuming.
25-years-old Angela was a big supporter of the #MeToo movement. She read and shared women’s stories on social media. One day, while reading another story, she had a thought about how horrible it would be to be a sexual predator. Since that day, she makes sure to stay away from other people in the subway and in other crowded places. She spends a lot of time reviewing her days and trying to be certain she did not cause inappropriate sexual contact. She now tries to never go out alone so that she has somebody else with her (a “witness”) to reassure her that she didn’t touch another person on the street.
The issue with the cases above is that these experiences did not cause OCD. They may have influenced the content of the person’s obsessions, but the predisposition to sticky intrusive thoughts most likely existed prior to these occurrences.
Finding the cause rarely has a significant impact on the treatment. Some people spend years doing “deep therapy” but they rarely find the “root,” and even if they do, the treatment is still the same.
You may never know what “caused” or triggered your OCD. The good news is that you can still get effective treatment and significantly improve your life.
Be very careful if your therapy involves searching for the origin of your OCD. It is much easier to engage in this kind of therapy than to do exposures that can be unpleasant. But then the therapy becomes just another avoidance behaviour where you invest effort and energy in not facing the real problem.
2. Examining the Evidence that Supports or Disproves the Thoughts
This is a legitimate CBT technique called Automatic Thoughts Record. You write down all the evidence that supports the thought, then you write down all the evidence that doesn’t support it and after that, you come up with a more balanced, realistic thought that is supposed to reduce your distress.
But it doesn’t reduce your distress. Not in the long term. The reason for that is that your OCD doesn’t concentrate on logic or reality. It zooms in on a possibility. And anything is, of course, possible. OCD then makes this tiny possibility look like a huge probability.
Thought records don’t work for OCD because when you are anxious, you concentrate not on how unlikely something is to happen, but on how horrible it will be if it happens.
To make matters worse, this technique often leads to an increase of two very common compulsions -- the “figuring it out” compulsion and the reassurance-seeking compulsion. So, definitely a no-go for OCD treatment – you have enough compulsions, why create more?
3. Working on Stopping the Obsessions
This is, of course, what every person with OCD wants – to stop the obsessions from entering their mind. If it was possible, that would be amazing! Unfortunately, there is no way to keep the thoughts from being generated by your brain. The only things that you can stop are engaging with these thoughts and performing the compulsions.
Still, there is a lot of misinformation out there about strategies for thought-stopping, such as rubber band snapping, screaming “Stop!” when you have an intrusive thought, replacing a “bad” thought with a “good” one, using distractions, or reciting positive affirmations.
Some people with OCD actually have a compulsion of suppressing their thoughts (one of my clients calls it a “self-induced amnesia”). Again, the last thing we want to do in treatment is to create more compulsions.
Photo: Turning Point Psychological Services
Alas, these thought-stopping strategies are like a Chinese finger trap – the one where you stick your finger in and then try to pull it out. The harder you pull, the more your finger becomes stuck. Similarly, the more you try to get rid of your thoughts, the more importance you give them and the “stickier” they become.
4. Working on Anxiety Reduction
This one sounds so good. And you hear about it everywhere. There are endless resources on the internet for anxiety reduction and numerous books are devoted to that too.
The problem is, attempts to get rid of anxiety lead to placing even greater significance on the anxiety. When you are trying hard to be anxiety-free, you reinforce the belief that anxiety is dangerous and intolerable. This, in turn, feeds the anxiety. The less we are willing to experience anxiety, the higher the anxiety will be. Just like trying to stop the obsessions makes the obsessions stronger, trying to get rid of anxiety increases it. What we resist, persists.
Anxiety is a natural response to a perceived threat, and we can’t override it by learning some quick tricks. We can’t really fool our sympathetic nervous system that evolved to keep us safe from real dangers. But what we can do is learn not to let anxiety control our lives.
When we allow ourselves to experience anxiety, fear, disgust, discomfort, or distress without performing the compulsions, we give ourselves an opportunity to discover that these emotions may be unpleasant, but they are not intolerable. As a good side effect to doing this, anxiety does diminish more often than not, but this cannot be the goal of our treatment -- otherwise it will backfire.
You can read more about how anxiety operates here: https://www.turningpointpsychology.ca/blog/how-anxiety-and-fear-work
5. Breathing, Meditation, Relaxation, and Positive Thinking
These techniques are closely related to anxiety reduction, but I decided to outline them separately as they are very prevalent in treatment. These techniques sound very legitimate and healthy. And they are, on one condition: they should not be used as “safety behaviours” for anxiety reduction.
So if you want to start or end your day with these practices – more power to you. You may feel more grounded and experience more calmness and clarity throughout the day.
But practice those as a response to your obsessions – and very quickly they turn into compulsions and reinforce your OCD. Therefore, we do not incorporate these strategies into our OCD treatment.
One exception is mindfulness meditation. This is a very specific type of meditation that does not involve relaxation. Its goal is to allow the thoughts and images to come and go without engaging with them or trying to get rid of them.
6. Receiving Supportive Reassurance
“Well, isn’t this what the therapist is for?” you may ask, -- “To support? To kindly reassure?” There is even a term – supportive counselling, which many therapists use when describing their therapeutic approach.
Bad news: No, OCD treatment cannot be described as supportive counselling.
More bad news: Reassurance is one of the most common compulsions in all OCD types. If the therapist is constantly reassuring you with the purpose of making you feel better, it means that he or she is co-compulsing with you. It will make you feel better during the session. And, it also will make your OCD stronger in the long run.
Good news: You don’t need reassurance to overcome your OCD. In therapy, you will learn to be self-compassionate and to support yourself in this difficult battle with OCD, while taking a very active approach to rebelling against it.
More good news: The therapist will be supportive without resorting to reassurance. He or she will also teach you how to support yourself in this difficult process of rebelling against OCD and how to do it without seeking reassurance or engaging in self-reassurance.
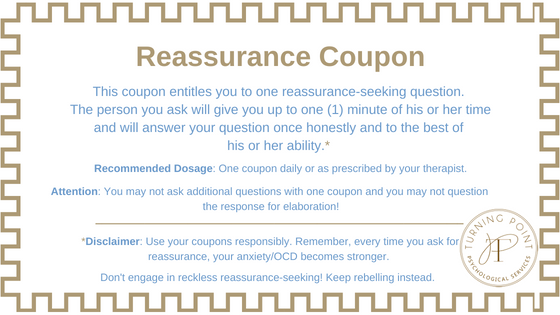
To start addressing your reassurance-seeking right away, you can print out these reassurance coupons and limit yourself to 8 coupons per week. Please read the instructions for using the coupons here.
7. Creating Numerous Exposure Hierarchies
An exposure hierarchy is a list of anxiety-triggering situations that are arranged in order of severity so that you can start facing these situations without resorting to compulsions.
You and your therapist may create a few informal hierarchies initially just to get the idea of how exposure works. But for many OCD sufferers, who have a massive variety of obsessions and compulsions, numerous hierarchies just become overwhelming.
To make matters worse, it is very common for obsessions and compulsions to change, so creating hierarchies feels like playing a never-ending whack-a-mole game (you can read more about it here).
In a traditional ERP approach, exposure exercises are structured in such a way that you start from the items on the list that make you just a little bit anxious and gradually progress to more difficult items. But, new research indicates that the best way to do exposure is to address the items on the list that vary in their degree of difficulty – in no specific order. Our clinical experience is consistent with that, so you will be encouraged to practice various exposures without concentrating too much on structuring them according to the level of difficulty.
In general, exposure hierarchy is a very helpful technique and if you are trying to cope with your OCD on your own, this is a great place to start. It’s just important to keep in mind that, especially in the case of numerous compulsions, it becomes too time-consuming and less effective.
Instead, it is imperative to really change your relationship with anxiety, to consistently rebel against your compulsions, and to practice all kinds of focused exposure as frequently as possible.
8. Rating Your Anxiety or Distress
What? But isn’t it a well-known CBT strategy?
Rating and re-rating your anxiety is just another way of focusing on it. Aren’t you giving it too much attention already? It’s like giving extra attention to a misbehaving child. Not worth it. The anxiety may be mild, moderate, or strong. The goal of the treatment is to help you make choices to take steps toward living a rich, full, and meaningful life regardless of the severity of anxiety.
9. Aiming to Lower Your Anxiety During Exposure in Order to Habituate to the Fear-Inducing Trigger
This is related to rating the anxiety as described in #8 and general anxiety reduction described in #4. The rating of SUDs (Subjective Units of Distress) is often done with the goal of reducing the anxiety during the exposure. This is done to monitor whether a habituation – getting used to the threatening external or internal trigger – takes place. It’s like getting used to the cold water in a swimming pool. After a few minutes you get used to the cold. Similarly, we can habituate to things we fear.
As stated at the beginning of this article, while exposure used to focus on anxiety reduction in the past, we now know that it is not necessary
The new emerging research shows that there are other mechanisms, not just habituation that underlie the effectiveness of exposure. One of the latest researches and treatment directions concentrates on creating a new neural pathway in your brain – the non-fearful pathway. To cultivate this new pathway, you need to practice your exposure in a variety of situations and under a variety of conditions. The conditions may include practicing exposure in different places, different situations, with different people, and in different moods.
The more you use your new neural pathway, the stronger it will become and the more likely you will be using this healthy pathway in difficult times.
So, if you practice ERP and your fear goes down – great. And if it doesn’t, but you still don’t do the rituals – even better! This is the situation where a lot of learning occurs. You learn that you can have a high level of fear and still not do the compulsion. Congratulations! Your new healthy neural pathway is becoming more established.
So, at our clinic, we won’t do the strategies above. What will we do instead? Click here to read about our iRebel approach to the treatment of OCD.
Have you been in therapy for OCD? Have you recognized some effective or ineffective strategies? Share your story in the comments below and help other OCD sufferers get the right treatment!
To learn more about anxiety and effective ways of dealing with it in the long-term, read our anxiety blog.
If you enjoyed this article, follow us on Facebook for more great tips and resources!
Anna Prudovski is a Psychologist and the Clinical Director of Turning Point Psychological Services. She has a special interest in treating anxiety disorders and OCD, as well as working with parents.
Anna lives with her husband and children in Vaughan, Ontario. When she is not treating patients, supervising clinicians, teaching CBT, and attending professional workshops, Anna enjoys practicing yoga, going on hikes with her family, traveling, studying Ayurveda, and spending time with friends. Her favorite pastime is reading.
-
Anxiety
- Jul 5, 2020 Anxiety and Related Disorders
- Jun 2, 2020 Panic Disorder
- Jul 7, 2019 Social Anxiety Disorder: Facts, Symptoms, Treatment, and Tips for Managing It.
- Jun 6, 2019 10 Popular Therapy Strategies that Don’t Work for Bad Anxiety or OCD
- Mar 6, 2019 10 Tips for Dealing with Anxiety
- Feb 7, 2019 Don’t Feed the Dinosaurs or How to Face Your Anxiety
- Jan 22, 2019 Meet Anxiety. Anxiety: Part 1/7
- Dec 24, 2018 Why does Anxiety Interfere with My Life So Much? Anxiety: Part 2/7
- Dec 17, 2017 Anatomy and Physiology of Anxiety. Anxiety: Part 3/7
- Dec 3, 2017 Dealing with Anxiety Components One by One. Anxiety: Part 4/7
- Nov 12, 2017 The Discovery of Oz the Terrible. Anxiety: Part 5/7
- Oct 8, 2017 Meet Your New Best Friend: Uncertainty. Anxiety: Part 6/7
- Sep 10, 2017 Some More Strategies to Help You Deal With Anxiety and Worry. Anxiety: Part 7/7
-
OCD & Co.
- Nov 23, 2021 Acceptance and Commitment Therapy (ACT) for OCD
- Sep 13, 2021 Relationship OCD (ROCD) and Its Treatment
- Jul 12, 2021 Existential OCD
- Jun 8, 2021 Real Event OCD and 10 Steps to Getting Better
- Apr 17, 2021 Signs That You or Someone You Know May Have OCD and Not Realize It
- Dec 2, 2020 Don’t Argue With a Brain Glitch. (10 Do's and 5 Don'ts for Parents of Kids with OCD)
- Sep 25, 2020 Do I have OCD? 8 Surprising OCD Myths
- Aug 15, 2020 9 Surprising Things We Don’t Do When Treating OCD at Our Clinic
- May 21, 2020 Illness Anxiety and How to Overcome It
- Feb 21, 2020 OCD and Online Romance Scam
- Jun 6, 2019 10 Popular Therapy Strategies that Don’t Work for Bad Anxiety or OCD
- Nov 17, 2018 Is it Possible to Be “a Little OCD?”
- Oct 23, 2018 Defeating the (Seemingly) Indestructible OCD Hydra: 8 Effective Tricks to Deal with New Obsessions.
- Oct 22, 2018 OCD, is That You Again? How to Know if Your New Thought is OCD, and 6 Concrete OCD-Repelling Strategies for You to Start Practicing Right Away.
- Oct 21, 2018 Trich or treat? Are you secretly pulling your hair out? Trichotillomania and its Treatment
- Apr 26, 2017 Stepping Off the OCD Hamster Wheel. A Therapist's Recovery Journey
- Parenting
-
Psychology
- Aug 21, 2019 The Road to ‘Stuckness’ is Paved with Good Intentions
- Sep 4, 2018 Having Difficulty Making Decisions? This Subtle Shift in Your Perspective May Change the Way You Approach Decisions from Now On.
- Aug 17, 2018 A Gentleman in Moscow or How to Live Life
- Jul 1, 2018 Who Goes to Therapy? Myths Versus Reality: The Therapist’s Perspective
- May 1, 2018 Do you often ask this innocent question? Watch out – you may be at risk for depression, anxiety, and other disorders.
- Feb 3, 2018 An effective hack to instantly take the edge off a negative emotion